Chapter 19: What are the Health Benefits of Regular Physical Activity?
Ian Janssen

Learning Objectives
By the end of this chapter, you should be able to:
- Recognize different types of study designs that are used to examine the relationship between physical activity and health.
- Explain the historical developments in research examining the relationship between physical activity and health.
- Describe the benefits of physical activity for reducing the risk of several chronic disease and premature mortality within adult populations.
- Illustrate the dose-response relationship between physical activity and mortality and risk for chronic disease.
- Argue for the health benefits of vigorous activities.
- Explain how different physical activity patterns can influence health.
- Describe the benefits of physical activity for health within children and youth.
- Summarize the Canadian physical activity guidelines.
Key Terms
accelerometer, bone mineral density, cancer, cardiorespiratory fitness, cardiovascular disease, chronic disease, coronary heart disease, cross-sectional study, dementia, dose-response relationship, experimental study, fracture, ground reaction forces, joint reaction forces, physical activity, meta-analysis, moderate intensity physical activity, musculoskeletal fitness, obesity, observational studies, physical activity, osteoporosis, prospective cohort study, randomized controlled trial, risk factor, stroke, type 2 diabetes, vigorous intensity physical activity.
Case Study: Research Approach to Study Health Benefits
In this chapter, a case study is not presented. As seen in the other chapters of this book, case presentations are very useful when examining how engagement in physical activity triggers a given physiological response and how these physiological responses vary from one person to the next. The relationship between physical activity and a given health outcome is not as clear cut as there is no guaranteed health response for a specific person. Rather than looking at individual responses when describing the relationship between physical activity and health, risks of specific health outcomes are compared in large groups of people who have varying physical activity levels. For instance, a researcher may examine whether a greater proportion of a group of inactive people die over a 10-year prior by comparison to similar group of physically active people. Therefore, the health benefits of physical activity in this chapter are illustrated by comparing health outcomes in groups of people with varying physical activity and fitness levels. Several examples have been drawn from the literature.
The Need to Study the Influence of Physical Activity on Health
Participation in moderate intensity and vigorous physical activity has been a major factor in the evolution of the human species. Humans emerged in conditions that required a high level of habitual physical activity, and an individuals’ fitness played a significant role in their ability to survive. Hunting, gathering of food and other necessities, and escaping animal predators were necessary parts of daily life for our ancient ancestors. The most physically fit had an advantage in these activities and were more likely to have survived and passed on their genes to the next generation. Thus, survival of humankind over tens of thousands of years required high levels of physical activity and performance.
Humans began to live in larger settlements around 10,000 BC with the advent of agricultural farming. At this time, the necessity for the majority of the population to engage in moderate intensity physical activity on a habitual basis continued. This remained the case until the industrial revolution in the latter half of the 18th century. The industrial revolution reflected a gradual transition from an agricultural–based economy towards a machine and manufacturing-based economy. After the start of the industrial revolution, technological progress continued to gain momentum with the development of steam-powered ships, the internal combustion engine, and electrical power. Over time, people enjoyed and became extremely reliant on these power sources. By the end of the industrial revolution survival of mankind was no longer contingent upon the majority of the population performing demanding physical work.
In the past century, technology continued to develop at an accelerated rate. Personal computers, fibre optics, communication satellites, the World Wide Web and a host of other inventions have changed the way we work and travel. Currently, jobs in the workplace and at home and transportation from one place to another rely even less on muscle power than they did only a generation ago (Church et al., 2011). Unless people make an intentional effort to engage in physical activity in their leisure time, it is unlikely that they will accumulate even modest amounts of moderate and physical activity. In fact, as much as 85-90% of the Canadian adult population do not accumulate 150 minutes per week of MVPA – this is less than 30 minutes of MVPA on a typical day (Colley et al., 2011). The focus of this chapter will be to discuss how the low physical activity levels within the population are having a negative influence on their health. Specifically, this chapter explains how a lack of MVPA is a risk factor for premature mortality and several chronic disease.

Chronic disease refer to diseases that are long-lasting or recurrent. The three leading causes of death in Canada (cancer, diseases of the heart, and cerebrovascular diseases), which combined account for 6 in 10 deaths, are all chronic diseases (Statistics Canada, 2018). A lack of physical activity, particularly MVPA, hereafter referred to as physical inactivity, contributes to all three of these leading causes of death. Approximately 15% of breast cancers, 24% of colon cancers, 25% of strokes, and 27% of heart attacks in Canadian adults could be avoided if 100% of the population engaged in an appropriate amount of MVPA (Janssen, 2012). In addition to being a risk factor for the leading causes of death, physical inactivity is associated with a host of other chronic diseases and conditions, including but not limited to, obesity, diabetes, osteoporosis, physical disability, anxiety, depression, and dementia (Warburton et al., 2010; 2018 Physical Activity Guidelines Advisory Committee, 2018).
Research Design: How the Relationship between Physical Activity and Health is Evaluated
This section provides an explanation of the research study designs that are used by researchers to assess the relationship between physical activity, chronic disease risk, and mortality risk. These relationships can be assessed using observational studies and experimental study designs. In observational studies researchers collect, record, and analyze data on study participants, but they do not intervene on the participants. That is, the physical activityof the participants is not controlled in any way by the researchers. For example, the participants may complete a questionnaire about their physical activity habits and the researchers will examine whether their reported level of MVPA is related to their future development of a chronic disease. Experimental studies involve some intervention or control of the participants’ physical activity levels by the researchers. For example, the participants may be invited into a laboratory 3 times per week over 4 months where they engage in an exercise program that is prescribed and monitored by the researchers. The researchers then determine whether this exercise program impacts the participants’ health or measurable risk factor for chronic disease.
Observational Studies
Two types of observational studies are commonly used in physical activity and health research: cross-sectional studies and prospective cohort studies. In cross-sectional studies the physical activity and health variables are measured at the same point in time and the researchers examine whether the variables are related. To demonstrate how a cross-sectional study would be conducted and interpreted, consider the following case, which is illustrated in Figure 21-1. Within a sample of 100 men, physical activity and blood pressure were measured. The 50 participants with the lowest MVPA levels were placed within the Inactive Group while the 50 participants with the highest MVPA levels were placed into the Active Group. Based on the blood pressure measures, participants were considered to have hypertension (blood pressure >140/90 mm Hg) or a normal blood pressure (blood pressure <140/90 mm Hg). Ten of the 50 participants in the Inactive Group, or 20%, had hypertension. Five of the 50 participants in the Active Group, or 10%, had hypertension. Therefore, the likelihood of having hypertension was 100% higher in the Inactive Group by comparison to the Active Group ((20% – 10%) / 10%) 100).
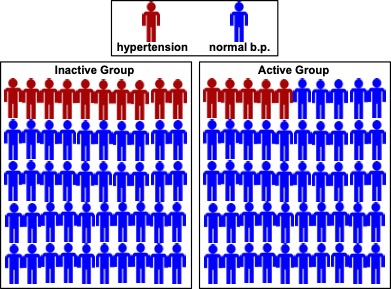
As the likelihood of having hypertension was increased in the Inactive group in this cross-sectional study, we can say that physical activity was related or associated to hypertension. However, because this is a cross-sectional study design, we do not know if physical inactivity preceded the development of hypertension or whether hypertension proceeding the development of inactivity. We can only tell that the two variables are related to each other at a specific point in time. Thus, based on this cross-sectional study we could not imply that a lack of MVPA caused hypertension. In order for physical activity to be considered a cause of the health outcome, there must be evidence from the other study designs that are described below.
The second type of observational study, prospective cohort study, begins by measuring the physical activity level in a group of participants. This is often referred to the baseline period. At the baseline period the participants must not have the health outcome that is being studied. Participants are then tracked into the future, in what is often called the follow-up period, to see who develops the health outcome or chronic disease. A finding that a greater proportion of the inactive participants develop the chronic disease during the follow-up period implies that physical inactivity precedes the chronic disease, thereby providing some evidence of a causal relationship.
To demonstrate how a prospective cohort study would be conducted and interpreted, consider the following case, which is illustrated in Figure 19-2. Within a sample of 100 men without hypertension, MVPA was measured at baseline and participants were placed into the Inactive Group (least active 50 participants) and the Active Group (most active 50 participants). The participants were then tracked over 10 years, and after the 10-year follow-up was completed, their blood pressure was measured to determine whether or not they had developed hypertension in the follow-up period. Twenty percent (10 out of 50) of the Inactive Group developed hypertension compared to 10% (5 out of 50) of the Active group, indicating that the risk of developing hypertension was 100% higher in the Inactive Group.
Experimental Studies
While prospective cohort studies provide some evidence of a causal relationship, experimental studies provide an even stronger form of causal evidence. The experimental study design that is used most commonly in the physical activity and health research field is referred to as a randomized controlled trial. In this type of study, the participants are randomly allocated (e.g. name drawn out of hat) into a control group and one or more experimental group. The health outcome of interest is measured at baseline in all participants, who are then randomized into the different groups. After randomization, the experimental group(s) undergoes the physical activity intervention, while the control group is not provided with an intervention and is asked to maintain their normal physical activity level. After the intervention is completed, the health outcome is measured again in a follow-up exam to see if greater improvements occurred in the experimental group(s) relative to the control group.
To illustrate the randomized controlled trial design, consider a study that examines whether aerobic exercise and/or resistance improves systolic blood pressure. A total of 99 inactive women with hypertension are recruited into the study. Blood pressure is measured in all participants who were then randomly assigned into a Control Group (N = 33), an aerobic Exercise Group (N = 33), or a Resistance Exercise Group (N = 33). Over the next 3 months, the Control Group engaged in no exercise, the Aerobic Exercise Group engages in 150 minutes per week of aerobic exercise, and the Resistance Group engages in 150 minutes per week of resistance exercise. The exercise interventions were prescribed and monitored by the research team. After the 3-month intervention was completed, the blood pressure of all 99 participants was measured again and the change in blood pressure from the baseline to follow-up exam was determined for each participant. The average change in blood pressure can be compared statistically across the three groups to compare the effects of the physical activity interventions.
Historical Perspectives on Physical Activity and Health
The modern history of physical activity and health research began in the 1950’s with the work of Dr. Jeremy Morris who studied the development of coronary heart disease in British workers using a prospective cohort design (Morris et al., 1953). Specifically, he found that a group of highly active double-decker bus conductors, who spent the majority of their day on their feet and climbed the stairs on the bus numerous times, had a 30% lower risk of having a heart attack during a two-year follow-up than a group of sedentary bus drivers. Dr. Morris later reported that postmen had a lower risk of developing coronary heart disease than sedentary office clerks and telephone operators (Morris and Crawford, 1958).
Evidence of the health benefits of physical activity continued to build in the latter half of the 20th century. Dr. Ralph Paffenbarger made a number of important contributions. Most notably amongst Dr. Paffenbarger’s studies were those based on the alumni of Harvard University. The men who participated in his studies completed a comprehensive physical activity questionnaire and were followed for coronary heart disease, using a prospective cohort study. In his seminal paper published in 1978, Dr. Paffenbarger noted that the amount of stairs climbed, blocks walked, strenuous sports plhttps://kinesiology.ucalgary.ca/macintosh/glossary/pha-tend#prospective-cohort-study-ayed, and total physical activity energy expenditure all reduced coronary heart disease risk (Paffenbarger et al., 1978). Compared to men with a physical activity energy expenditure above 2000 calories per week, men with a physical activity energy expenditure below 2000 calories per week were 64% more likely to have developed coronary artery disease during the follow-up period. This 1978 publication provided some of the first evidence that participation in physical activity – physical activity performed outside of the occupational setting – has protective effect on chronic disease risk.

In the 1980’s, important developments in the discipline were made with the research of Dr. Steven Blair and colleagues from the Cooper Institute in Dallas, Texas. These researchers assembled the Aerobics Center Longitudinal Study, a prospective cohort of over 13,000 adults. Rather than measuring physical activity, this research team h ad their study participants complete a maximal treadmill test to measure their cardiorespiratory (Blair et al., 1989). In addition to genetics, MVPA performed in recent weeks and months is an important determinant of fitness so, to a certain extent, fitness is an objective measure of physical activity.
Prior to Dr. Blair’s work, research in the field, such as the studies conducted by Dr. Paffenbarger, relied on subjective measures of physical activity that were obtained by questionnaire. Objective measures of fitness, such as those obtained in the Aerobic Centre Longitudinal Study, provide additional insight into the contribution of physical activity to good health. The initial findings from Dr. Blair and colleagues prospective cohort study were quite striking (Blair et al., 1989). By comparison to the most fit men (top 20th percentile), the least fit men (lowest 20th percentile) had a 244% greater risk of dying during the follow-up period. Similarly, compared to the most fit women, the least fit women had a 365% greater risk of dying during the follow-up period. Note how strong these risks are for low fitness (measured objectively) in comparison to those for physical inactivity (measured subjectively) observed by Paffenbarger and colleagues (Paffenbarger et al., 1978) in the Harvard Alumni Study. One of the consequences of using imprecise measurement techniques, which is typical of subjective measures of physical activity obtained by questionnaire, is that the relationship between physical activity and health that the researchers report on within their research paper will be weakened by comparison to what the true relationship is. In other words, the true association between physical activity and the health outcome may be underestimated when physical activity is measured using a physical activity questionnaire, which is typical of most of the published studies in this field. Thus, the way in which physical activity is measured should be considered when interpreting the associations between physical activity and health. Recent prospective cohort studies have, for the first time, looked at the association between objective measures of MVPA, as determined with an accelerometer, and health outcomes. As expected, these studies found very strong associations between MVPA and health. For instance, Borgundvaag and Janssen reported that mortality risk was increased by over 400% in the least active group by comparison to the most active group when MVPA was measured with an accelerometer (Borgundvaag and Janssen, 2017). Conversely, a review of studies that used questionnaire measures of MVPA suggested that physical inactivity was only associated with a 35% increased risk of mortality (Warburton et al., 2010).
There has been an infusion of randomized controlled trial in recent years. These randomized controlled trials have typically been fairly small in size (<100 participants), have focused on risk factor (e.g. blood pressure, bone mineral density) and not disease outcomes (e.g. heart disease, osteoporosis), and have not been as rigorously conducted as the randomized controlled trials conducted in clinical and medical research disciplines. Thus, the strength of the experimental studies in the physical activity sciences has traditionally been weak in comparison to those conducted in clinical medicine. However, since the turn of the century, large and well-controlled, randomized lifestyle based interventions have been conducted that meet the most rigorous standards (Tuomilehto et al., 2001; Diabetes Prevention Program Research Group, 2002). Consider, for instance the Finnish Diabetes Prevention Study (Tuomilehto et al., 2001). The 552 study participants were randomly assigned to an intervention group or a control group. The intervention group received individual counselling aimed at reducing weight, increasing physical activity, and improving diet. After four years, 23% of the participants in the control group had developed diabetes, which was more than double the 11% figure noted in the intervention group.
Relationships between Physical Activity and the Risk of Mortality and Chronic Disease
The next section of this chapter summarizes the relationship between physical activity with premature mortality and several important chronic disease. Example studies from the literature have been selected to highlight some of the key findings and issues. There have been entire chapters, and in some cases books, that cover the relationships that are discussed in a few paragraphs in this chapter. Table 21.1 summarizes the extent of the risk for premature mortality and several chronic conditions for the average physically inactive individual compared with the average physically active individual.
Table 21-1 Risks for premature mortality and chronic disease associated with physical inactivity
|
Condition |
Extent of increased risk in physically inactive individuals |
|
Premature mortality |
↑↑ |
|
Cancer |
↑ |
|
Cardiovascular disease |
↑↑ |
|
Type 2 diabetes |
↑↑↑ |
|
Osteoporosis |
↑↑↑ |
|
↑↑ |
|
|
Poor health |
↑↑↑ |
↑Risk for condition increased by approximately 1-24%; ↑↑ risk for condition increased by approximately 25-49%; ↑↑↑ risk for condition increased by 50% or more.
Physical Activity and Mortality
More than 100 prospective cohort studies have examined whether physical activity reduces the risk of premature mortality. The finding from these studies indicate that most active individuals experience about a 30% reduction in the risk of dying during follow-up compared to the least active individuals (Warburton et al., 2010; 2018 Physical Activity Guidelines Advisory Committee, 2018). The protective effects of physical activity extend to both sexes, adults of different ages, and to different racial and ethnic groups (Warburton et al., 2010; 2018 Physical Activity Guidelines Advisory Committee, 2018). Findings from one study suggest that about 1 in 6 deaths are attributable to a physically inactive lifestyle and that physically inactive people live an average of 3 years shorter than active people (Paffenbarger et al., 1986).
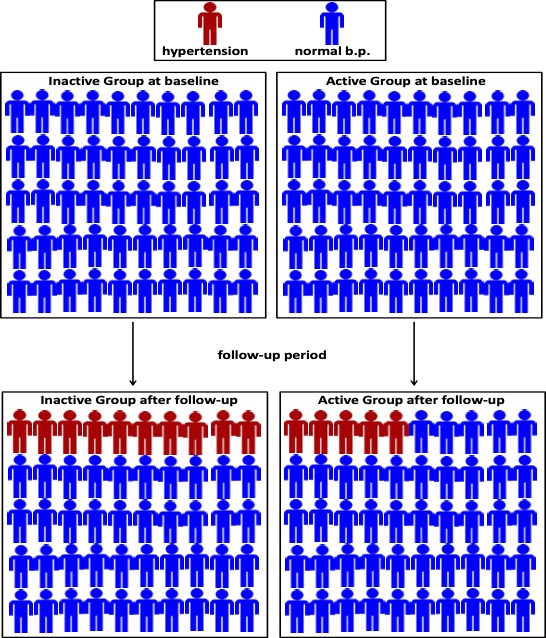
The pattern of the relationship between the weekly duration of MVPA and mortality risk is shown in Figure 19-3. This figure was generated from the findings of an 8-year prospective cohort study of over 400,000 Taiwanese adults (Wen et al., 2011). This figure shows how there are large differences in mortality risk between individuals who are inactive compared to those with low activity levels, and more modest differences in mortality risk between those with high activity compared to those with very high activity levels. About 70% of the total benefits that MVPA has on mortality risk occur within the first 150 minutes per week (2018 Physical Activity Guidelines Advisory Committee, 2018).
Walking is the most common form of physical activity among adults. Several studies have examined the influence of walking on mortality risk (Siegel et al., 1995). Walking for at least 2 hours per week is associated with a reduced risk of premature mortality. Consider findings from the Copenhagen City Heart Study, a prospective cohort of 7308 healthy men and women followed over 12 years (Schnohr et al., 2007). Compared to men who walked <½ hour per day and who walked at a slow pace, men who walked >2 hour per day at a slow pace had a 57% reduction in mortality risk. In addition to the duration of physical activity, additional findings from the Copenhagen City Heart Study indicate that the intensity is also important. Specifically, compared to men who walked > 2 hours per day and who walked at a slow pace, men who walked >2 hour per day at a fast pace had a 35% reduction in mortality risk.
There is also strong and consistent evidence that cardiorespiratory is inversely related to mortality risk. One study examining the relation between cardiorespiratory fitness and mortality was based on a follow-up of the 1981 Canada Fitness Survey (Villeneuve et al., 1998). Within this sample of 7916 Canadian adults, an undesirable cardiorespiratory fitness level, as determined using the Canadian aerobic fitness step test, was associated with a 52% increased risk of death.
Physical Activity and Cardiovascular Disease
Within Canada about one third of all deaths are caused by cardiovascular disease (Statistics Canada, 2018). Cardiovascular disease is the leading cause of hospitalizations in Canada, with about 14% of all hospitalizations being caused by cardiovascular disease (Statistics Canada, 2008).
A vast scientific literature has examined the role that physical activity and cardiorespiratory play in the risk of cardiovascular disease. From these studies it can be concluded that physical inactivity and low cardiorespiratory fitness are causally linked to an increased risk of several forms of cardiovascular disease including coronary heart disease and stroke (Kohl, 2001). Higher physical activity and physical activity levels both have a protective effect on cardiovascular disease risk (Kohl, 2001).
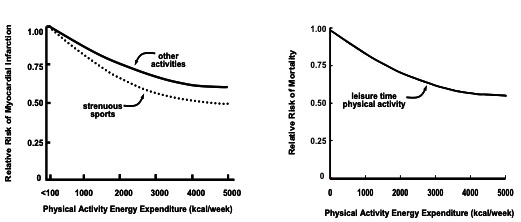
The pattern of the relationship between physical activity and cardiovascular disease risk indicates that as physical activity levels get increasingly higher, cardiovascular disease risk continues to decrease (Kohl, 2001). A typical example of this pattern is illustrated in the left panel of Figure 19-4. This figure shows an inverse, curvilinear association between total weekly physical activity energy expenditure – whether it be strenuous sports or other non-vigorous activities – and the risk of having a heart attack (Paffenbarger et al., 1978). This figure is based on findings from the Harvard Alumni Study that was discussed in Section 3 of this chapter.

As with coronary heart disease, a high physical activity and fitness level are causally linked to a decreased risk of stroke. A meta-analysis, which summarized the evidence from all of the published studies, indicated that relative to inactive individuals, moderately active individuals have a 17% reduction in stroke risk and highly active individuals have a 25% reduction in stroke risk (Lee et al., 2003).
In addition to providing protection against the development of cardiovascular disease, engagement in physical activity is important in the management of poor health and the prevention of mortality in individuals with existing cardiovascular disease (Jolliffe et al., 2001; Thompson et al., 2003). A prospective cohort study of 1,045 elderly men and women with coronary heart disease indicated that baseline physical activity was related to all-cause mortality risk over a 9 year follow-up period (Janssen and Jolliffe, 2006), as illustrated in the right panel of Figure 19-4. Note how the curvilinear pattern of the relation between physical activity and cardiovascular disease risk in healthy adults (left panel in Figure 19-4) is similar to the pattern of the relation between physical activity and mortality risk in adults with cardiovascular disease (right panel in Figure 19-4). Hopefully you have started to see an emerging theme about the relationship between physical activity and health – there are very large health benefits when comparing inactive individuals with even moderately active individuals, but further increases in activity level have progressively less impacts on chronic disease and mortality risk.
Physical Activity and Cancer
Cancer has overtaken cardiovascular disease as the leading cause of death in Canada (Canadian Cancer Statistics Advisory Committee, 2018; Statistics Canada, 2018). Over 200,000 new cases of cancer and 80,000 deaths from cancer occur in Canada each year (Canadian Cancer Statistics Advisory Committee, 2018). The 5 most common cancer sites are skin, prostate gland, lung, colon/rectum, and breast (Canadian Cancer Statistics Advisory Committee, 2018).
Risk factors for cancer can be non-modifiable (e.g. age, sex, race) or modifiable and can vary by the site of the cancer. There are several modifiable risk factors for cancer such as tobacco, exposure to too much ionizing radiation and too much sunlight, a poor diet (e.g. lack of fruits and vegetables), obesity, and physical inactivity and low fitness. Some risk factors, such as physical inactivity and low fitness, are associated with more than one form of cancer and thereby impact overall cancer rates and deaths. For instance, results from the Aerobics Center Longitudinal Study indicate that, within adults who were cancer free at the start of the study, the risks for dying from any form of cancer during the follow-up period decreased with increasing levels of cardiorespiratory (Farrell et al., 2007). Specifically, compared to unfit men, the risk of dying from cancer was reduced by 33% in moderately fit men and by 51% in highly fit men.
Studies of physical activity including occupational physical activity have demonstrated that physical activity is associated with reduced risk for colon cancer (Lee, 2007). Individuals engaging in aerobic physical activity for 3 to 4 hours per week at a moderate intensity or vigorous intensity have a 30% reduction in the risk of developing colon cancer. A dose-response relationship also is apparent, with risk decreasing at higher levels of physical activity.
There is consistent evidence that routine participation in physical activity provides protection against breast cancer, particularly within postmenopausal women. Consider the findings from the American Association of Retired Persons Diet and Health Study (Peters et al., 2009). This prospective cohort study followed 182,862 postmenopausal women over 7 years, during which time 6,609 women developed breast cancer. Compared to women who never engaged in activity, the risk of developing breast cancer was reduced by 8% in women who were active 3-4 times per week and by 15% in women who were active 5 or more times per week.
While the earliest studies of physical activity and cancer risk primarily focused on colon and breast cancer, more recent work has examined other cancer sites. In addition to colon and breast cancer, there is now strong and consistent evidence demonstrating that increased participation in MVPA is associated with an approximately 10% to 25% reduction in the risk of developing bladder cancer, endometrial cancer, esophageal cancer, gastric cancer, renal cancer, and lung cancer (2018 Physical Activity Guidelines Advisory Committee, 2018). Limited evidence indicates that MVPA is associated with small reductions in the risk of head and neck cancer, hematologic cancers, ovarian cancer, pancreatic cancer, and prostate cancer (2018 Physical Activity Guidelines Advisory Committee, 2018). Researchers have also considered whether physical activity provides health benefits for individuals who have been diagnosed with cancer (Newton and Galvao, 2008). The results from both observational and experimental studies indicate that participation in physical activity following cancer diagnosis can reduce cancer symptoms, help manage the side effects and outcomes of cancer treatment (surgery, radiation and chemotherapy), improve health, maintain physical function, and reduce fat gain and muscle and bone loss (Newton and Galvao, 2008). Furthermore, regular physical activity post-diagnosis increases survivorship by about 50% (Newton and Galvao, 2008).
Physical Activity and Type 2 Diabetes
More than 3 million Canadians live with diabetes, with about 90% of these being cases of diabetes (Canadian Diabetes Association, 2012). Type 2 diabetes increases the risk of cardiovascular disease, renal disease, cancer, blindness, and physical and mental disability. Life expectancy is reduced by 5 to 10 years in people with type 2 diabetes.
Physical activity and low cardiorespiratory are strong risk factor for the development of diabetes in both men and women. Results from the Nurses Health prospective cohort study will be used to highlight these associations (Hu et al., 1999). In an 8-year follow-up of 70,102 women from the Nurses Health Study who had no history of diabetes, the risk of developing type 2 diabetes was reduced by 25% in moderately active women and by 46% in highly active women. Interestingly, among Nurses Health Study participants who did not perform physical activity, the risk of developing type 2 diabetes w as reduced by 27% in women who walked a modest amount and by 42% in women who walked a lot. The dose-response relationship is further illustrated in Figure 19-5 (left panel).
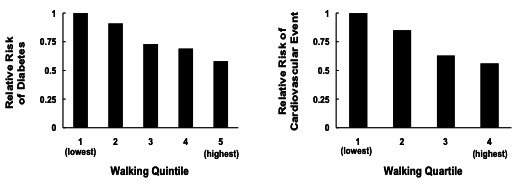
Additional results from the Nurses Health Study suggest that physical activity provides protection against the development of chronic disease within adults with diabetes (Hu et al., 2001). Hu and colleagues examined a subset of 5125 women from the Nurses Health Study who had diabetes at baseline. Over a 14-year follow-up period, the risk of developing cardiovascular disease was about 50% lower in the most active (top 25th percentile) diabetic women compared to the least active (lowest 25th percentile) diabetic women. Similarly, the diabetic women who walked the most (top 25th percentile) reduced their risk of developing cardiovascular disease by about 50% compared to the diabetic women who walked the least (lowest 25th percentile). The relationship between walking and the risk of cardiovascular disease in diabetic participants who did not perform physical activity is illustrated in Figure 19-5 (right panel).
Physical Activity and Obesity

About 1 in 4 Canadian adults have obesity and about 1 in 10 Canadian children and youth have obesity (Statistics Canada, 2018). Obesity results from a chronic energy imbalance whereby intake exceeds expenditure; physical inactivity therefore plays an important role in the obesity problem. Results from cross-sectional and prospective cohort studies have shown, in general, that physical activity is related to obesity such that physically active individuals are less likely to have and develop obesity in comparison to inactive individuals (Ross and Janssen, 2001; Ross and Janssen, 2007; 2018 Physical Activity Guidelines Advisory Committee, 2018).
There has been considerable debate about the amount of physical activity required to prevent weight gain throughout adulthood. In 2002, the Institute of Medicine recommended that adults should accumulate 60 to 90 minutes of physical activity on a daily basis to prevent unwanted weight gain (Food and Nutrition Board (Institute of Medicine), 2003). In 2003, the International Association for the Study of Obesity suggested that for most adults 45-60 minutes of moderate intensity per day would be sufficient to prevent unwanted weight gain (Saris et al., 2003). The 2018 Physical Activity Guidelines for Americans scientific report concluded that attenuation of weight gain is most pronounced when MVPA exceeds 150 minutes per week (2018 Physical Activity Guidelines Advisory Committee, 2018). Thus, the volume of physical activity needed for the prevention of weight gain is higher than the volume of physical activity needed to prevent chronic disease and premature mortality.
The role of physical activity as a treatment strategy for obese individuals has received considerable attention. Early reviews of the literature suggested that increasing physical activity in the absence of caloric restriction through diet was only associated with a 1-2 kg weight loss (National Institutes of Health National Heart Lung and Blood Institute, 1998). However, few of the earlier weight loss studies prescribed a volume of physical activity that would have resulted in a meaningful energy expenditure (Ross and Janssen, 2001). For example, Mourier and colleagues conducted an 8-week randomized controlled trial in a group of 21 overweight patients with diabetes (Mourier et al., 1997). Participants in the intervention group completed 3 aerobic exercise sessions per week, each session lasting 45 minutes at 75% of V̇O2max. This 8-week exercise program would have resulted in a total energy expenditure of ~6700 calorie. Given that 1 kg of fat contains 7700 calories of energy, the expected weight loss from this physical activity intervention would have been slightly less than 1 kg over the 8-week intervention (assuming diet remained calorie-neutral). Thus, the fact that participants in the intervention group only lost an average of 1.5 kg in this study is not surprising given the modest amount of physical activity prescribed. In other words, while 135 minutes per week of moderate intensity has a significant impact on many of the other health outcomes discussed in this chapter, based on the laws of thermodynamics, this volume of physical activity would only have a minimal effect on body fat and weight.
The results from some randomized controlled trial have indicated that physical activity in the absence of a calorie restricted diet can be associated with significant weight loss if the duration of physical activity is sufficient. For instance, Ross and colleagues demonstrated that moderately obese men and women lost about 7% of their body weight over a 3 to 4 month period by engaging in approximately 60 minutes of moderate aerobic physical activity on a daily basis, primarily in the form of brisk walking, in the absence of changes in caloric intake (Ross et al., 2000; Ross et al., 2004).
Physical Activity and Osteoporosis
Osteoporosis related fracture are common amongst older adults. In fact, at least 1 in 3 women and 1 in 5 men will suffer from an osteoporosis related fracture during their lifetime (Osteoporosis Canada, 2017). Two million Canadians are affected by osteoporosis and over 80% of fractures in people aged 50 or older are attributable to osteoporosis (Osteoporosis Canada, 2017).
Early understanding about the benefits of physical activity on the risk of developing osteoporosis was generated from cross-sectional studies (Borer, 2005). The results from these studies suggested that athletes in sports that include running, jumping, and other weight bearing activities (e.g. soccer, running, basketball, weight lifting) have higher bone mineral density (BMD) values than non-athletes. Conversely, athletes in sports that do not involve running and jumping (e.g. swimming, speed skating, cross-country skiing) have comparable BMD values as non-athletes.
Mineral and bone mass increase throughout growth and maturation and peak at around age 20. From about age 20 to age 50, bone loss tends to occur very slowly, at a rate of less than 0.5% per year. Evidence from several randomized controlled trial has demonstrated that prolonged exercise interventions that involve either ground reaction force (e.g. running, jumping) or joint reaction force (e.g. weight training) increase BMD in young adults (Borer, 2005). For example, one randomized controlled trial prescribed 8 months of weight training or running to female college students (Snow-Harter et al., 1992). The weight training consisted of 3 sessions per week of 3 sets of 10 exercises. Participants in the running group ran 7-17 km per week at 75% of their maximal heart rate. Bone mineral density in the lumbar spine region improved by about 1.3% in both the weight trainers and runners in response to the 8-month exercise interventions. These may seem like trivial changes in bone mineral density but recall that bone loss during the early adult years is very slow at <0.5% per year. Thus, these 8-month exercise programs would have reversed approximately 3 years of bone mineral loss in the young women who participated in the study. Over the long term, this may have delayed or prevented the development of osteoporosis in these women as they aged.
After age 50, bone mineral loss is accelerated, particularly in women. Postmenopausal women tend to lose between 1-2% of their bone mass each year. Exercise involving ground reaction force or joint reaction force is an effective strategy for reducing and even reversing age-related loss in bone mineral content in older adults (Borer, 2005). In one 11 month long experimental study of 39 women aged 65 years, a ground reaction force exercise program (jogging, walking, stairs) increased total body mineral by 2% (Kohrt et al., 1997). Similarly, a joint reaction force exercise program (weight training, rowing) increased in bone mineral density by 1.6% (Kohrt et al., 1997).
Limited research has considered whether engagement in physical activity helps prevent the transition into a diseased state of osteoporosis, and most of the existing studies have focused on the occurrence of osteoporotic fractures. Consider the following two examples. First, a 20 year prospective cohort study of men aged 50 years and older (Kujala et al., 2000). In this study, men who participated in physical activity were only one third as likely to have a hip fracture during the follow-up period in comparison to men who did not participate in vigorous physical activity. Second, a 4 year prospective cohort study of elderly women (Cummings et al., 1995). In this study, women who walked for exercise in the baseline exam had a 30% lower risk of having a hip fracture during the follow-up than women who did not walk for exercise. The results from these studies confirm that physical activity, particularly when vigorous in nature, provides some protection against the risk of osteoporosis and related fractures.
Physical Activity and Mental Health
Physical activity is associated with several measures of health including mood, anxiety, depression, and cognitive function. The benefits of physical activity on mental health include acute or post-recovery effects from a single session of exercise, chronic effects from engaging in regular physical activity over many weeks and months, the prevention of mental health disorders (e.g. development of depression or dementia), and improving mental health within persons suffering from a mental health disorder.
Strong evidence demonstrates that bouts of physical activity, when performed at an intensity that exceeds the lactate or ventilatory threshold, can result in immediate improvements in mood (Oliveira et al., 2015). Similarly, a meta-analysis of 36 RCTs concluded that participating in a 20-30 minute long bout of MVPA improves symptoms of anxiety such as feelings of apprehension, fear, worry, and nervousness (Ensari et al., 2015). Literature reviews that have compared the effects of exercise to other treatments have reported that exercise is just as effective, or perhaps even more effect, as standard care treatment for anxiety (Wegner et al., 2014; Ensari et al., 2015).
Observational studies provide evidence that physical activity protects against the onset of depression and its symptoms. In the published prospective cohort studies the risk of developing depression symptoms was reduced by approximately 50% among active adults compared to inactive adults (Physical Activity Guidelines Advisory Committee, 2018). Although the minimal, optimal, and type of physical activity needed to protect against the development of depression and its symptoms is not known, it is clear that the volume of physical activity is related to depression in a dose-response manner such that increasing benefits occur with more activity. In one prospective cohort study of 1,947 community-dwelling adults aged 50 and older, the risk for developing depression was 131% lower in the moderately active group and 395% lower in the highly active group in comparison to the group with the lowest activity levels (Strawbridge et al., 2002). Interestingly, within that study the effect of inactivity on the risk of developing depression was greater than the effect of any of the other risk factor considered including age, gender, financial status, neighbourhood problems, education, and disability status.
Participation in physical activity is associated with improved scores on neurophysiological tests that assess processing speed, memory, and executive function (2018 Physical Activity Guidelines Advisory Committee, 2018). Physical activity also delays the onset of cognitive decline and the incidence of dementia by about 40% (2018 Physical Activity Guidelines Advisory Committee, 2018). It is encouraging that moderate intensity that most older adults are capable of performing, such as walking, have a protective effect. In one prospective cohort study of 2,257 physically capable men aged 71 to 93 years, men who walked the least (<0.25 miles per day) had an 80% higher risk of developing dementia than men who walked the most (>2 miles per day) (Abbott et al., 2004).

In addition to being an effective preventive measure, physical activity is a useful treatment strategy for individuals with health problems. A meta-analysis of 14 randomized controlled trial that were conducted on people diagnosed with depression reported that the mean reduction in depression symptoms was equivalent to 1 standard deviation of the mean score for those measures (Lawlor and Hopker, 2001). It is also encouraging that the effects of routine physical activity on symptoms within depressed individuals are equivalent to those of drug therapy (Blumenthal et al., 2007). As with depression, a meta-analysis of 10 randomized controlled trails of older adults with cognitive impairments concluded that physical activity interventions provided meaningful benefits to cognitive function (Heyn et al., 2004).
Physical Activity and Functional Health
This section reviews evidence related to the effects of physical activity on simple functional activities within middle-aged and older adults. Examples of functional activities considered in this section include the ability to walk at a normal speed on a flat surface, climb a flight of stairs, perform basic activities of daily living (e.g. bathing, dressing, grooming), and perform activities that enable one to live independently (e.g. shopping, travel in community, light housework).
Prospective cohort studies have consistently shown that middle-aged and older adults who participate in regular physical activity, particularly aerobic activity, have a reduced risk of developing functional limitations in the order of 30% (2018 Physical Activity Guidelines Advisory Committee, 2018). Furthermore, greater amounts of physical activity are associated with lower risks than modest amounts of activity. There is also evidence that changes in physical activity influence subsequent disability risk. Specifically, a prospective cohort of 549 older adults were studied annually from 1984 to 2000 (Berk et al., 2006). Four groups were formed depending on their physical activity level during the baseline and annual follow-up visits: Sedentary (low activity at baseline and during follow-up), Exercise Increasers (low activity at baseline and high activity during follow-up), Exercise Decreasers (high activity at baseline and low activity during follow-up), and Exercisers (high activity at baseline and during follow-up). Over the 16-year follow-up, the increase in the disability index score was far greater in the Sedentary (+0.37) and Exercise Decreasers (+0.27) than in the Exercise Increasers (+0.17) and Exercisers (+0.11). These are encouraging findings which indicate that physical activity, even when begun later in life, can help postpone the onset of physical disability.
Regular physical activity in older adults with existing functional limitations improves their functional ability. The majority of the published experimental study have included both aerobic and strengthening activities in the interventions (Physical Activity Guidelines Advisory Committee, 2018). For this reason, physical activity programs aimed at improving health in older adults with pre-existing functional limitations reflects a pattern of physical activity that involves 30-90 minutes of MVPA performed on 3-5 days per week, in which most of this time is devoted to aerobic and strengthening activity, with a shorter amount of time spent on other forms of activity such as flexibility and balance (Physical Activity Guidelines Advisory Committee, 2018).
Gender Feature
Physical Activity Improves Health in Both Genders
MVPA levels are different in men and women such that the average man accumulates more MVPA over a week than the average women. Data in a nationally representative sample of Canadian adults, in which physical activity was measured objectively over one week using accelerometers, indicates that the average Canadian man accumulates 27 minutes per week of MVPA and that the average Canadian women accumulates 21 minutes per week of MVPA (Colley et al., 2011). While 23% of Canadian men achieve the guideline for MVPA (e.g. at least 150 minutes of MVPA accumulated in bouts of at least 10 minutes), only 17% of Canadian women do (Colley et al., 2011). Chronic disease and premature mortality risks are also different in men and women. At any given age men have a higher risk of dying and developing coronary heart disease and stroke than women. Conversely, at any given age women have a higher risk of developing osteoporosis, health problems, and health problems.
Although MVPA levels, premature mortality risk, and the risk of many chronic diseases is different in men and women, participation in regular MVPA reduces the risk of premature mortality and chronic disease risk irrespective of gender. Furthermore, the strength of the relationships between MVPA, premature mortality, and chronic disease risk are remarkably comparable in men and women. Put another way, the health benefits of physical activity are similar in men and women.
Resistance Training, Muscular Fitness, and Health
The relations between physical activity and fitness with health that have been covered so far in this chapter are, for the most part, based on aerobic and cardiorespiratory-based measures of physical activity and fitness. The protective effects of strength– or resistance-based physical activities and fitness have not been as well studied. Nonetheless, the available information suggests that these types of activity and fitness measures protect against many chronic disease and mortality risk. For instance, in the Health Professional’s Follow-up Study of over 40,000 men, those who reported participating in 30 minutes or more of weight training per week had a 23% reduction in coronary heart disease risk compared to those who performed no weight training (Tanasescu et al., 2002). A 19 year follow-up of 8,677 men from the Aerobics Center Longitudinal Study indicated that men within the lowest muscular strength group (lowest third) had a 64% higher risk of cancer mortality than men in the highest muscular strength group (top third) (Ruiz et al., 2009). A 13-year follow-up of 8,116 adults from the 1981 Canada Fitness Survey suggests that direct measures of musculoskeletal fitness provide some protection against mortality risk (Katzmarzyk and Craig, 2002). Take for example the sit-ups test (maximal number of sit-ups performed in 60 seconds). In comparison to the best performers, Canadian men and women in the lowest sit-ups quartiles were about 150% more likely to die during the follow-up period (Katzmarzyk and Craig, 2002).
Physical Activity and Heath in Children and Youth
Although not as plentiful as in adults, there is considerable knowledge about the health benefits of physical activity in school-aged children and youth. These studies have focused on risk factor (e.g. high blood pressure, obesity, symptoms of anxiety) that may already be present in the growing years, rather than on the disease outcomes (e.g. coronary heart disease) that do not occur until older ages. Many chronic disease take decades to develop and have their origins in childhood. Thus, it is important to study the relationship between physical activity and health within the pediatric population.
A systematic evaluation and meta-analysis of the existing studies linking physical activity to several risk factor in school-aged children and youth was published in 2010 (Janssen and Leblanc, 2010). This evaluation reached the following conclusions regarding the amount, intensity, and type of physical activity needed for health in this age group:
Amount of Physical Activity: There is strong and consistent evidence based on several risk factor (e.g. obesity, blood pressure, blood lipids, insulin resistance, BMD, measures of health) that participating in as little as 2 or 3 hours of MVPA per week is associated with health benefits. There is a dose-response relationship between physical activity and health in children and youth. Thus, there are differences in health measures between the least active and somewhat active young people, and also between somewhat active and highly active young people.
Intensity of Physical Activity: Moderate intensity and vigorous (MacIntosh et al., 2021) are associated with many health benefits. The available information suggests that vigorous intensity activities provide additional health benefits beyond moderate intensity activities. At present, there is a lack of evidence on the health benefits of low intensity activities.
Type of Activity: Many health outcomes responded almost exclusively to aerobic -type physical activities. However, BMD is more favourably affected by resistance and high-impact activities such as jumping exercises.
Research Feature
Physical Activity in Preschool Aged Children
A new area of research interest within the physical activity and health field is to discern the health benefits of physical activity for children younger than 5 years of age. Society has traditionally thought of the early years as being a time of life when children are habitually “active enough.” However, studies that have assessed the physical activity levels of preschool children using objective measures have reported MVPA levels that are much lower than what most people would expect.
Take for instance, a 2011 study of 30 preschool (3 to 5 years old) children from Ontario (Obeid et al., 2011). Children in this study wore accelerometers on their right hip for one week. These accelerometers detected and recorded the participants’ movement every 3 seconds. The results of this study indicated that, in a typical day, participants accumulated 219 minutes of physical activity. However, 66% of this activity was of a low intensity; only 21% was of a moderate intensity and only 14% was of a vigorous. Additional findings indicated that the 45 minutes per day of MVPA that the participants accumulated was extremely intermittent and sporadic in nature. In fact, 95% of the MVPA was accumulated in brief bursts of activity that were less than 15 seconds in length. Interestingly, there were no differences in light, moderate, or vigorous intensity physical activity levels in the boys and girls that were examined in this study. This suggests that gender differences in physical activity do not start at a young age.
A key strength to this study is the objective assessment of physical activity using accelerometers. In particular, the measurement of each 3 second time period over a full week allowed the researchers to measure the sporadic physical activity patterns of preschool aged children. A key limitation of this study is its small sample size. Larger and more diverse studies of preschool aged children are needed to gain a better understanding of the physical activity levels in this age group. Future research also needs to address the relationship between physical activity and health in preschoolers.
The period of life for which we know the least about the health benefits of physical activity is the early years. As part of a rigorous process to develop physical activity recommendations for the early years, a group of experts recently conducted a systematic review of the available studies to evaluate the relationship between physical activity and health indicators during the early years (Carson et al., 2017). This committee found evidence from observational studies that higher amounts of physical activity are consistently associated with favourable indicators of motor development, fitness, and bone and skeletal health. Furthermore, favourable associations were found for a variety of types of physical activity, including active play, aerobic activities, dance, and both organized and unstructured activities. For infants, more time spent in the prone position (i.e. tummy time) was associated with good health. More research in this age group is needed to determine the specific amount, intensity, frequency, or type of physical activity needed to promote good health.
Dose-Response Issues in Physical Activity and Health
Components of Physical Activity Dose
The primary components used to determine physical activity dose, or the total energy expended from physical activity, are duration and intensity. Physical activity is usually defined as being of a light, moderate intensity, or vigorous. As explained below, physical activity intensity can be defined in both relative and absolute terms.
Most exercise physiologists define physical activity intensity in relative terms. Relative intensity refers to the level of effort required by a person to do an activity relative to their own maximum. For instance, when using heart rate, moderate intensity, is defined as 50 to 69% of maximal heart rate while vigorous is defined as 70% or more of maximal heart rate.
Another way to express physical activity intensity is in absolute terms, which is the approach taken by most researchers who look at the relationship between physical activity and health. Absolute intensity refers to the absolute amount of energy used by the body per minute of activity, where 1.0 metabolic equivalent (MET) refers to resting energy expenditure. When using an absolute scale, moderate intensity activities refer activities from 3.0 to 5.9 MET s and vigorous refers to activities where the MET value is 6.0 or higher. This method of describing moderate to vigorous physical activity ignores the capabilities or fitness of the client (MacIntosh et al., 2021).
One way to sum up how much physical activity a person has accumulated over a week, or their dose of physical activity, is to calculate the energy expenditure based on the MET values and the duration of all activities performed. For instance, if a person performs 100 minutes of moderate intensity activity at 4 METs and 30 minutes of vigorous at 8.0 METs over a week, their weekly dose of physical activity is 640 MET minutes (100 4 + 30 8) or 10.7 MET hours (640 MET minutes / 60 minutes per hour).
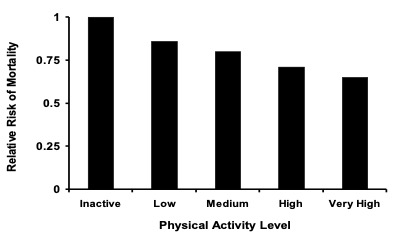
Higher intensity activities appear to have a beneficial effect on some health outcomes independent of the physical activity dose (Paffenbarger et al., 1978; Hu et al., 1999; Manson et al., 2002). Consider the example illustrated in Figure 19-6. This example is explained in greater detail in the Highlight Box. This figure comes from a cross-sectional study of American adults (Janssen and Ross, 2012). Within that study, a given amount of energy expended from vigorous was associated with a greater reduction in the prevalence of the metabolic syndrome than a corresponding amount of energy expended from moderate intensity activity.
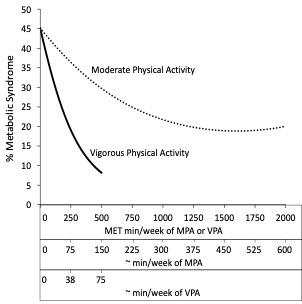
Estimated prevalence of the metabolic syndrome according to energy expenditure (minutes per week) of physical activity (MPA) and physical activity (VPA). In addition to the energy expenditure, the approximate times needed to accumulate the energy expenditure for moderate and vigorous activity are also shown on the x-axis. Figure taken from reference (Janssen and Ross, 2012).
Highlight Feature: Physical Activity Intensity Impacts Health
In this cross-sectional study of 1,841 adults, the authors used accelerometers to measure physical activity over 7 consecutive days (Janssen and Ross, 2012). The data recorded from the accelerometers was used to estimate the energy expenditure from physical activity (3.0 – 5.9 MET s) and from physical activity (≥ 6.0 METs). In addition to wearing the accelerometers for one week, participants had their waist circumference measured, their blood pressure taken, and a fasting blood sample drawn. Triglyceride, high density lipoprotein (HDL)-cholesterol, and glucose levels were measured in the fasted blood samples. Participants who had 3 or more of the following risk factor were considered to have metabolic syndrome: high waist circumference (men ≥ 94 cm, women ≥ 80 cm), high triglycerides (≥ 1.7 mmolL-1), low HDL-cholesterol (men < 1.0 mmolL-1, women < 1.3 mmolL-1), elevated blood pressure (systolic pressure ≥ 130 mm Hg or diastolic pressure ≥ 85 mm Hg or use of hypertension medication), and elevated glucose (≥ 5.6 mmolL-1 or diagnosed diabetes) (Alberti et al., 2009). The metabolic syndrome is a clustering of cardiometabolic risk factors that increases cardiovascular disease, diabetes, and all-cause mortality risks (Ardern and Janssen, 2007).
The results from this study, which are further illustrated in Figure 21.6, show that energy expenditure from physical activity had a smaller impact on the metabolic syndrome than the same energy expended from physical activity. For instance, between 0 and 500 MET minutes per week of moderate intensity physical activity, the prevalence of the metabolic syndrome risk decreased by 15%. While between 0 and 500 MET minutes per week of vigorous physical activity, the prevalence of the metabolic syndrome decreased by 37%. To accumulate 500 MET minutes, one would have to engage in about 150 minutes of moderate physical activity and only 75 minutes of vigorous physical activity. Thus, within this study half the duration of vigorous physical activity produced double the health benefit. Furthermore, the benefit obtained from moderate intensity physical activity elicits no further benefit after about 1200 MET minute.
The second main component of physical activity dose, duration, is a function of the session duration and frequency of participation in activity. Results of experimental studies that evaluated the effect of a single longer bout of activity (e.g. a single 30 minute session) to the effect of three or four shorter bouts of activity performed across the day (e.g. three 10 minute sessions), performed on several days per week, indicate that performing multiple shorter bouts produced changes in fitness and risk factor for cardiovascular disease and diabetes that are quite similar to those produced by the single longer bout (Hardman, 2001). For example, in a randomized controlled trial of 50 overweight women, 30 minutes of brisk walking performed in a single session on 5 days·wk-1 resulted in a 14% increase in V̇O2max and a 7% loss in weight; while 30 minutes of brisk walking accumulated in 3 sessions on 5 days·wk-1 resulted in a 16% increase in V̇O2max and a 9% loss in weight (Jakicic et al., 1995).
Observational study that have used accelerometers to assess physical activity on a minute-by-minute basis over 7 full days have considered whether MVPA accumulated in intervals as short as one minute can benefit health, as long as enough of this sporadic or intermittent physical activity is accumulated over the course of the day. These studies have found that when the total duration of physical activity is matched, sporadic or intermittent physical activity is associated with the same health benefits as longer bouts of physical activity (2018 Physical Activity Guidelines Advisory Committee, 2018). For instance, in a cross-sectional sample of Canadian adults, each additional MET -hour per week of MVPA was associated with a 10% decrease in the likelihood of having the metabolic syndrome irrespective of whether that MVPA was accumulated in one or two bouts of physical activity lasting at least 10 minutes or through many short spurts of sporadic physical activity (Clarke and Janssen, 2014).
Another question to ask is whether a person should accumulate their suggested weekly dose of physical activity over several days of the week, or whether a couple of longer sessions performed on 1 or 2 days would be acceptable. Consider, for instance, the “weekend warrior” who is quite active, but who compresses all of their weekly activity into the weekend. Is this a healthy pattern of physical activity? A recent study addressed this question by comparing the benefits of the weekend warrior pattern of physical activity to the benefits of a regularly active pattern of physical activity where participants were active on at least 3 days of the week (O’Donovan et al., 2017). In this study both physical activity patterns were associated with a reduced risk of cancer, cardiovascular disease, and mortality. Furthermore, the risk reductions were very comparable in the weekend warrior and regularly active groups. This suggests that the total amount of physical activity accumulated over the week is important while the pattern of accumulation is not.
Minimal and Optimal Amounts of Physical Activity
A large proportion of the population would like to know the minimal amount of physical activity needed to produce meaningful health benefits. This likely depends on a person’s current physical activity level. A person who has been at complete bed rest may benefit just from getting out of bed for a few minutes each day. Some of the research presented in this chapter suggests that a small amount of walking, even at a light pace, can reduce mortality risk in very inactive individuals with a chronic disease such as diabetes. Unfortunately, few studies have carefully considered the minimal amount of physical activity needed for good health in the general public. Nonetheless, the associations between physical activity and various health outcomes, as illustrated in Figures 19-3 through 19=6, indicate that only a modest amount of moderate intensity is required to bring about meaningful benefits for many health outcomes. This is perhaps best reflected from the findings of a study of over 400,000 Taiwanese adults. This study found that individuals who accumulated 90 minutes per week of MVPA, which averages out to only 15 min per day, had a 14% reduced risk of mortality and had a 3 year longer life expectancy compared to individuals who accumulated no MVPA (Wen et al., 2011).
Similar to the issues around defining the minimal amount of physical activity needed for health, it is unclear as to what point an increase in physical activity provides no further health benefits. The plateau may also vary by health outcome – it may be quite low for some health outcomes and quite high for others. For instance, there is a linear relation between miles run and HDL-cholesterol levels that does not plateau even at 80 miles run per week (Williams, 1997). This suggests that continued health benefits, at least for some variables, can be achieved even after running 10 hours per week at a vigorous pace. Although health benefits may not completely level off at high activity levels, there are certainly diminishing returns once a moderate level of physical activity is reached (2018 Physical Activity Guidelines Advisory Committee, 2018).
Translation of Research Findings into Public Health Recommendations
Recommendations for Fitness and Health
Scientific understanding of the health benefits of physical activity is of little relevance if this information cannot be translated to the general public so they can apply this to their lives to improve their health. In recent decades there has been increasingly growing efforts to develop public health messages, through physical activity guidelines, about the appropriate amount, intensity, frequency, and type of physical activity needed for good health. These guidelines have been developed by experts in the field who were tasked with synthesizing the findings from the scientific literature and applying the information to create messages that can be clearly communicated to the public.
The first endorsed recommendations for physical activity were those of the ACSM. In their 1975 exercise guidelines book (American College of Sports Medicine) and 1978 position statement (American College of Sports Medicine), the ACSM recommended that people engage in exercise on 3-5 days of the week for 15-60 minutes at an intensity of 50-85% V̇O2max. These recommendations were geared towards the appropriate exercise for developing and maintaining fitness in healthy adults. They were not geared towards health outcomes. For two decades after the ACSM guidelines were developed, physical activity guidelines continued to focus on the appropriate exercise for fitness. This changed in 1995 with the publication of the U.S. Centers for Disease Control (CDC) and the ACSM recommendation on physical activity and public health (Pate et al., 1995). This recommendation was intended to communicate to the general public how much and what types of physical activity are needed to maintain good health. The following recommendation was issued by the panel: “Every U.S. adult should accumulate 30 minutes or more of moderate intensity on most, preferably all, days of the week”. Since these initial public health recommendations for physical activity and health, several other organizations and countries have developed their own recommendations. Canada’s most recent guidelines and recommendations for physical activity are discussed in the following few paragraphs (Tremblay et al., 2011; Tremblay et al., 2016; Tremblay et al., 2017). Note that the recommendations for children of the early years (0-4 years) and school-aged children and youth (5-17 years) are no longer contained within a stand along physical activity guideline. Rather, the physical activity recommendations for these age group are now included within 24-hour movement behaviour guidelines. These 24-hour guidelines also include recommendations for sedentary behaviour and sleep, which are not discussed here. Copies of Canada’s physical activity and 24-hour movement guidelines and their accompanying recommendations and promotional materials can be downloaded for free at http://www.csep.ca/guidelines.
The Early Years (0-4 years)
●Infants (< 1 year): Be physically active several times a day in a variety of ways, particularly through interactive floor-based play—more is better. For those not yet mobile, this includes at least 30 minutes of tummy time spread throughout the day while awake.
●Toddlers (1-2 years): At least 180 minutesd–1 of a variety of physical activities at any intensity, including energetic play, spread throughout the day—more is better.
●Preschoolers (3-4 years): At least 180 minutesd-1 spent in a variety of physical activities spread throughout the day, of which at least 60 minutes is energetic play—more is better.

School-Aged Children and Youth (5-17 years)
●Accumulate at least 60 minutes per day of physical activity involving a variety of aerobic activities. Vigorous physical activities, and muscle and bone strengthening activities should each be incorporated at least 3 days per week;
●Several hours per day of a variety of structured and unstructured light physical activities.
Adults (18-64 years)
●Accumulate at least 150 minutes of vigorous aerobic physical activity per week, in bouts of 10 minutes or more.
●It is also beneficial to add muscle and bone strengthening activities using major muscle groups, at least 2 days per week.
●More physical activity provides greater health benefits.
Older Adults (65 years and older)
●Accumulate at least 150 minutes of vigorous aerobic physical activity per week, in bouts of 10 minutes or more.
●It is also beneficial to add muscle and bone strengthening activities using major muscle groups, at least 2 days per week.
●Those with poor mobility should perform physical activities to enhance balance and prevent falls.
●More physical activity provides greater health benefits
Summary
In the current technologically driven society, the majority of the population is extremely inactive (Colley et al., 2011; Colley et al., 2017). Unfortunately, there is now clear and strong scientific evidence that, irrespective of age and gender, an inactive lifestyle is strongly and causally related with several measures of poor health. Because physical inactivity is a highly prevalent condition and because it has such a strong impact on chronic disease risk, a significant proportion of chronic disease in Canada is directly attributable to physical inactivity. In fact, about 1 in 4 cases of coronary artery disease, stroke, and colon cancer in Canada are caused by inactivity and about 1 in 3 cases of diabetes and osteoporosis are caused by inactivity (Janssen, 2012).
Systematic reviews of the literature and consensus meetings help by Canadian and international experts in the area of physical activity and health, have led to improved physical activity recommendations for Canadians of all ages (Tremblay et al., 2011; Tremblay et al., 2016; Tremblay et al., 2017). These guidelines indicate that to achieve substantial health benefits, adults and older adults should accumulate at least 150 minutes of MVPA on a weekly basis, school-aged children and youth should accumulate at least 60 minutes of MVPA on the average day, and children of the early years should accumulate at least 180 minutes of activity of any intensity on the average day. Activity levels above these cut- points will be associated with even greater health benefits.
Exercises or Topics for Discussion
Add Topics of Discussion
References
2018 Physical Activity Guidelines Advisory Committee. 2018. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC.
Abbott RD, White LR, Ross GW, Masaki KH, Curb JD, and Petrovitch H. 2004. Walking and dementia in physically capable elderly men. Journal of the American Medical Association 292(12):1447-1453.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, and Smith Jr SC. 2009. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640-1645.
American College of Sports Medicine. 1975. Guidelines for graded exercise testing and prescription. Philadelphia, PA, Lea & Febiger.
American College of Sports Medicine. 1978. Position statement – The recommended quantity and quality of exericse for developing and maintaining fitness in healthy adults. Medicine & Science in Sports & Exercise 10:vii-x.
Ardern CI and Janssen I. 2007. Metabolic syndrome and its association with morbidity and mortality. Applied Physiology, Nutrition, and Metabolism 32(1):33-45.
Berk DR, Hubert HB, and Fries JF. 2006. Associations of changes in exercise level with subsequent disability among seniors: a 16-year longitudinal study. Journal of Gerontology Series A – Biological Sciences and Medical Sciences 61(1):97-102.
Blair SN, Kohl 3rd HW, Paffenbarger Jr RS, Clark DG, Cooper KH, and Gibbons LW. 1989. Physical fitness and all-cause mortality. A prospective study of healthy men and women. Journal of the American Medical Association 262(17):2395-2401.
Blumenthal JA, Babyak MA, Doraiswamy PM, Watkins L, Hoffman BM, Barbour KA, Herman S, Craighead WE, Brosse AL, Waugh R, Hinderliter A, and Sherwood A. 2007. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosomatic Medicine 69(7):587-596.
Borer KT. 2005. Physical activity in the prevention and amelioration of osteoporosis in women: interaction of mechanical, hormonal and dietary factors. Sports Medicine 35(9):779-830.
Borgundvaag E and Janssen I. 2017. Objectively measured physical activity and mortality risk among American adults. American Journal of Preventive Medicine 52(1):e25-e31.
Canadian Cancer Statistics Advisory Committee. 2018. Canadian Cancer Statistics 2018. Toronto, ON.
Canadian Diabetes Association. 2012. The prevalence and cost of diabetes. Toronto, ON, Canadian Diabetes Association.
Carson V, Lee EY, Hewitt L, Jennings C, Hunter S, Kuzik N, Stearns JA, Unrau SP, Poitras VJ, Gray C, Adamo KB, Janssen I, Okely AD, Spence JC, Timmons BW, Sampson M, and Tremblay MS. 2017. Systematic review of the relationships between physical activity and health indicators in the early years (0-4 years). BMC Public Health 17(Suppl 5):854.
Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, Martin CK, Blair SN, and Bouchard C. 2011. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLOS One 6(5):e19657.
Clarke J and Janssen I. 2014. Sporadic and bouted physical activity and the metabolic syndrome in adults. Medicine & Science in Sports & Exercise 46(1):76-83.
Colley RC, Carson V, Garriguet D, Janssen I, Roberts KC, and Tremblay MS. 2017. Physical activity of Canadian children and youth, 2007 to 2015. Health Reports 28(10):8-16.
Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, and Tremblay MS. 2011. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Reports 22(1):7-14.
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, and Vogt TM. 1995. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. New England Journal of Medicine 332(12):767-773.
Diabetes Prevention Program Research Group. 2002. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine 346(6):393-403.
Ensari I, Greenlee TA, Motl RW, and Petruzzello SJ. 2015. Meta-analysis of acute exercise effects on state anxiety: An update of randomized controlled trials over the past 25 years. Depression and Anxiety 32(8):624-634.
Farrell SW, Cortese GM, LaMonte MJ, and Blair SN. 2007. Cardiorespiratory fitness, different measures of adiposity, and cancer mortality in men. Obesity (Silver Spring) 15(12):3140-3149.
Food and Nutrition Board (Institute of Medicine). 2003. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). Washington, DC, National Academies Press.
Hardman AE. 2001. Issues of fractionization of exercise (short vs long bouts). Medicine & Science in Sports & Exercise 33(6 Suppl):S421-427; discussion S452-423.
Heyn P, Abreu BC, and Ottenbacher KJ. 2004. The effects of exercise training on elderly persons with cognitive impairment and dementia: a meta-analysis. Archives of Physical Medicine and Rehabilitation 85(10):1694-1704.
Hu FB, Sigal RJ, Rich-Edwards JW, Colditz GA, Solomon CG, Willett WC, Speizer FE, and Manson JE. 1999. Walking compared with vigorous physical activity and risk of type 2 diabetes in women: a prospective study. Journal of the American Medical Association 282(15):1433-1439.
Hu FB, Stampfer MJ, Solomon C, Liu S, Colditz GA, Speizer FE, Willett WC, and Manson JE. 2001. Physical activity and risk for cardiovascular events in diabetic women. Annals of Internal Medicine 134(2):96-105.
Jakicic JM, Wing RR, Butler BA, and Robertson RJ. 1995. Prescribing exercise in multiple short bouts versus one continuous bout: effects on adherence, cardiorespiratory fitness, and weight loss in overweight women. International Journal of Obesity and Related Metabolic Disorders 19(12):893-901.Janssen I. 2012. Health care costs of physical inactivity in Canadian adults. Applied Physiology, Nutrition, and Metabolism 37(4):803-806.
Janssen I and Jolliffe CJ. 2006. Influence of physical activity on mortality in elderly with coronary artery disease. Medicine & Science in Sports & Exercise 38(3):418-417.
Janssen I and Leblanc AG. 2010. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. International Journal of Behavioral Nutrition and Physical Activity 7(1):40.
Janssen I and Ross R. 2012. Vigorous intensity physical activity is related to the metabolic syndrome independent of the physical activity dose. International Journal of Epidemiology 41(4):899-904.
Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, and Ebrahim S. 2001. Exercise-based rehabilitation for coronary heart disease. Cochrane Database of Systemic Reviews (1):CD001800.
Katzmarzyk PT and Craig CL. 2002. Musculoskeletal fitness and risk of mortality. Medicine & Science in Sports & Exercise 34(5):740-744.
Kohl HW 3rd. 2001. Physical activity and cardiovascular disease: evidence for a dose response. Medicine & Science in Sports & Exercise 33(6 Suppl):S472-483; discussion S493-474.Kohrt WM, Ehsani AA, and Birge SJ Jr. 1997. Effects of exercise involving predominantly either joint-reaction or ground-reaction forces on bone mineral density in older women. Journal of Bone and Mineral Research 12(8):1253-1261.
Kujala UM, Kaprio J, Kannus P, Sarna S, and Koskenvuo M. 2000. Physical activity and osteoporotic hip fracture risk in men. Archives of Internal Medicine 160(5):705-708.
Lawlor DA and Hopker SW. 2001. The effectiveness of exercise as an intervention in the management of depression: systematic review and meta-regression analysis of randomised controlled trials. BMJ 322(7289):763-767.
Lee CD, Folsom AR, and Blair SN. 2003. Physical activity and stroke risk: a meta-analysis. Stroke 34(10):2475-2481.
Lee I-M. 2007. Physical activity, fitness, and cancer. Physical Activity and Health. C. Bouchard, S. N. Blair and W. L. Haskell. Champaign, IL, Human Kinetics: 205-218.
MacIntosh, BR, Murias, JM, Kier, DA, and Weir, JM. What is moderate to vigorous physical activity? Frontiers in Physiology 12: 2021 https://doi.org/10.3389/fphys.2021.682233.
Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A, Perri MG, Sheps DS, Pettinger MB, and Siscovick DS. 2002. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. New England Journal of Medicine 347(10):716-725.
Morris JN and Crawford MD. 1958. Coronary heart disease and physical activity of work: Evidence of a national necropsy survey. BMJ 30:1485-1496.
Morris JN, Heady JA, Raffle PA, Roberts CG, and Parks JW. 1953. Coronary heart-disease and physical activity of work. Lancet 265:1053-1057, 1111-1120.
Mourier A, Gautier JF, De Kerviler E, Bigard AX, Villette JM, Garnier JP, Duvallet A, Guezennec CY, and Cathelineau G. 1997. Mobilization of visceral adipose tissue related to the improvement in insulin sensitivity in response to physical training in NIDDM. Effects of branched-chain amino acid supplements. Diabetes Care 20(3):385-391.
National Institutes of Health National Heart Lung and Blood Institute. 1998. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Obesity Research 6(S2):S51-210.
Newton RU and Galvao DA. 2008. Exercise in prevention and management of cancer. Current Treatment Options in Oncology 9(2-3):135-146.
O’Donovan G, Lee IM, Hamer M, and Stamatakis E. 2017. Association of “Weekend Warrior” and Other Leisure Time Physical Activity Patterns With Risks for All-Cause, Cardiovascular Disease, and Cancer Mortality. Journal of the American Medical Association Internal Medicine 177(3):335-342.
Obeid J, Nguyen T, Gabel L, and Timmons BW. 2011. Physical activity in Ontario preschoolers: prevalence and measurement issues. Applied Physiology, Nutrition, and Metabolism 36(2):291-297.
Oliveira BR, Deslandes AC, and Santos TM. 2015. Differences in exercise intensity seems to influence the affective responses in self-selected and imposed exercise: a meta-analysis. Frontiers in Psychology 6:1105.
Osteoporosis Canada. 2017. Impact Report 2017. Toronto, ON.
Paffenbarger RS Jr, Brand RJ, Sholtz RI, and Jung DL. 1978. Energy expenditure, cigarette smoking, and blood pressure level as related to death from specific diseases. American Journal of Epidemiology 108(1):12-18.
Paffenbarger RS Jr, Hyde RT, Wing AL, and Hsieh CC. 1986. Physical activity, all-cause mortality, and longevity of college alumni. New England Journal of Medicine 314(10):605-613.
Paffenbarger RS Jr, Wing AL, and Hyde RT. 1978. Physical activity as an index of heart attack risk in college alumni. American Journal of Epidemiology 108(3):161-175.
Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW, King AC, and et al. 1995. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. Journal of the American Medical Association 273(5):402-407.
Peters TM, Schatzkin A, Gierach GL, Moore SC, Lacey JV Jr, Wareham NJ, Ekelund U, Hollenbeck AR, and Leitzmann MF. 2009. Physical activity and postmenopausal breast cancer risk in the NIH-AARP diet and health study. Cancer Epidemiology, Biomarkers & Prevention 18(1):289-296.
Ross R, Dagnone D, Jones PJ, Smith H, Paddags A, Hudson R, and Janssen I. 2000. Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men. A randomized, controlled trial. Annals of Internal Medicine 133(2):92-103.
Ross R and Janssen I. 2001. Physical activity, total and regional obesity: dose-response considerations. Medicine & Science in Sports & Exercise 33(6 Suppl):S521-527; discussion S528-529.
Ross R and Janssen I. 2007. Physical activity, fitness, and obesity. Physical Activity, Fitness, and Health. C. Bouchard, S. N. Blair and W. L. Haskell. Champaign, IL, Human Kinetics: 173-189.
Ross R, Janssen I, Dawson J, Kungl AM, Kuk JL, Wong SL, Nguyen-Duy TB, Lee S, Kilpatrick K, and Hudson R. 2004. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obesity Research 12(5):789-798.
Ruiz JR, Sui X, Lobelo F, Lee DC, Morrow JR Jr, Jackson AW, Hebert JR, Matthews CE, Sjostrom M, and Blair SN. 2009. Muscular strength and adiposity as predictors of adulthood cancer mortality in men. Cancer Epidemiology, Biomarkers & Prevention 18(5):1468-1476.
Saris WH, Blair SN, van Baak MA, Eaton SB, Davies PS, Di Pietro L, Fogelholm M, Rissanen A, Schoeller D, Swinburn B, Tremblay A, Westerterp KR, and Wyatt H. 2003. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obesity Reviews 4(2):101-114.
Schnohr P, Scharling H, and Jensen JS. 2007. Intensity versus duration of walking, impact on mortality: the Copenhagen City Heart Study. European Journal of Cardiovascular Prevention & Rehabilitation 14(1):72-78.
Siegel PZ, Brackbill RM, and Heath GW. 1995. The epidemiology of walking for exercise: implications for promoting activity among sedentary groups. American Journal of Public Health 85(5):706-710.
Snow-Harter C, Bouxsein ML, Lewis BT, Carter DR, and Marcus R. 1992. Effects of resistance and endurance exercise on bone mineral status of young women: a randomized exercise intervention trial. Journal of Bone and Mineral Research 7(7):761-769.
Statistics Canada. 2008. CANSIM database. Retrieved September 1, 2008, from http://cansim2.statcan.ca/cgiwin/cnsmcgi.exe?Lang=E&CANSIMFile=CII\CII_1_E.htm&RootDir=CII/.
Statistics Canada. 2018. Table 13-10-0373-01: Overweight and obesity based on measured body mass index, by age group and sex. Retrieved December 4, 2018, from https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310037301.
Statistics Canada. 2018. Table 13-10-0394-01: Leading causes of death, total population, by age group. Retrieved December 4, 2018, from https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310039401.
Strawbridge WJ, Deleger S, Roberts RE, and Kaplan GA. 2002. Physical activity reduces the risk of subsequent depression for older adults. American Journal of Epidemiology 156(4):328-334.
Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, and Hu FB. 2002. Exercise type and intensity in relation to coronary heart disease in men. Journal of the American Medical Association 288(16):1994-2000.
Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, Marcus BH, Berra K, Blair SN, Costa F, Franklin B, Fletcher GF, Gordon NF, Pate RR, Rodriguez BL, Yancey AK, and Wenger NK. 2003. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation 107(24):3109-3116.
Tremblay MS, Carson V, Chaput J-P, Connor Gorber S, Dinh T, Duggan M, Faulkner G, Gray CE, Gruber R, Janson K, Janssen I, Katzmarzyk PT, Kho ME, Latimer-Cheung AE, Leblanc C, Okely AD, Olds T, Pate RR, Phillips A, Poitras VJ, Rodenburg S, Sampson M, Saunders TJ, Stone JA, Stratton G, Weiss SK, and Zehr L. 2016. Canadian 24-hour Movement Guidelines for Children and Youth : An integration of physical activity, sedentary behaviour, and sleep. Applied Physiology, Nutrition, and Metabolism 41:311-327.
Tremblay MS, Chaput JP, Adamo KB, Aubert S, Barnes JD, Choquette L, Duggan M, Faulkner G, Goldfield GS, Gray CE, Gruber R, Janson K, Janssen I, Janssen X, Jaramillo Garcia A, Kuzik N, LeBlanc C, MacLean J, Okely AD, Poitras VJ, Rayner ME, Reilly JJ, Sampson M, Spence JC, Timmons BW, and Carson V. 2017. Canadian 24-Hour Movement Guidelines for the Early Years (0-4 years): An Integration of Physical Activity, Sedentary Behaviour, and Sleep. BMC Public Health 17(Suppl 5):874.
Tremblay MS, Warburton DE, Janssen I, Paterson DH, Latimer AE, Rhodes RE, Kho ME, Hicks A, Leblanc AG, Zehr L, Murumets K, and Duggan M. 2011. New Canadian physical activity guidelines. Applied Physiology, Nutrition, and Metabolism 36(1):36-46.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, Salminen V, and Uusitupa M. 2001. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. New England Journal of Medicine 344(18):1343-1350.
Villeneuve PJ, Morrison HI, Craig CL, and Schaubel DE. 1998. Physical activity, physical fitness, and risk of dying. Epidemiology 9(6):626-631.
Warburton DE, Charlesworth S, Nettlefold L, Ivey A, and Bredin SS. 2010. A systematic review of the evidence for Canada’s physical activity guidelines for adults. International Journal of Behavioral Nutrition and Physical Activity 7(1):39.
Wegner M, Helmich I, Machado S, Nardi AE, Arias-Carrion O, and Budde H. 2014. Effects of exercise on anxiety and depression disorders: review of meta-analyses and neurobiological mechanisms. CNS & Neurological Disorders – Drug Targets 13(6):1002-1014.
Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, Chan HT, Tsao CK, Tsai SP, and Wu X. 2011. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet 378(9798):1244-1253.
Williams PT. 1997. Relationship of distance run per week to coronary heart disease risk factors in 8283 male runners. The National Runners’ Health Study. Archives of Internal Medicine 157(2):191-198.
About the Author
Ian Janssen, School of Kinesiology & Health Studies and the Department of Public Health Sciences, Queens University, Kingston, ON, Canada

Dr. Janssen received his PhD in Exercise Physiology from Queen’s University in 2002 at which time he was awarded the Governor General’s Academic Gold Medal for his thesis research. Dr. Janssen completed his postdoctoral training at Tufts University and Queen’s University. In 2004, Dr. Janssen was hired as a faculty member under the Queen’s National Scholars program. He is currently a Professor and the Canada Research Chair in Physical Activity and Obesity in the School of Kinesiology & Health Studies and the Department of Public Health Sciences at Queen’s University. He teaches undergraduate courses in research methods as well as physical activity and health. His research program focuses on the surveillance, determinants, outcomes, and measurement of physical inactivity and their associated health risks. He has published more than 300 peer-reviewed papers and book chapters in these topic areas.