82 Plasma Cell Myeloma (Multiple Myeloma)
Michelle To and Valentin Villatoro
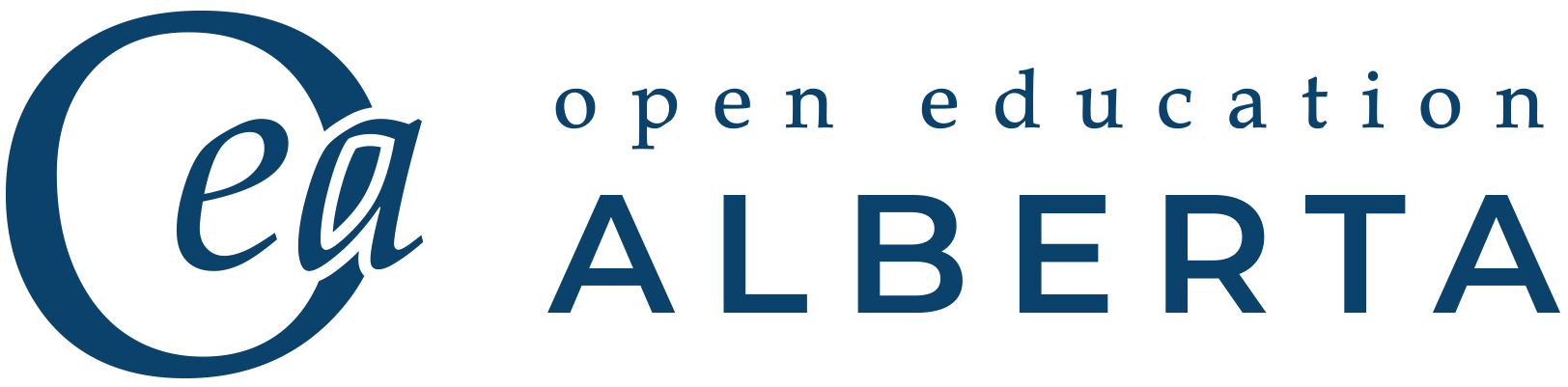
- An image from a peripheral blood smear demonstrating rouleaux, which is a characteristic finding of plasma cell myeloma. 50x oil immersion. From MLS Collection, University of Alberta, https://doi.org/10.7939/R3833ND55
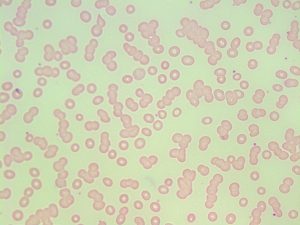
- An image from a peripheral blood smear demonstrating rouleaux, which is a characteristic finding of plasma cell myeloma. 50x oil immersion. From MLS Collection, University of Alberta, https://doi.org/10.7939/R3CZ32M1F
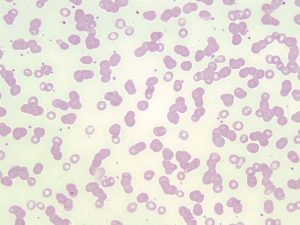
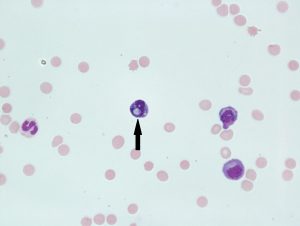
- An image from a bone marrow direct smear in a patient with plasma cell myeloma demonstrating a plasma cell. Note the perinuclear clearing surrounding the nucleus, and basophilic cytoplasm. 100x oil immersion. From MLS Collection, University of Alberta, https://doi.org/10.7939/R3VM43C6D
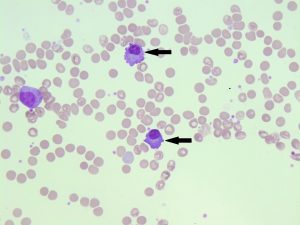
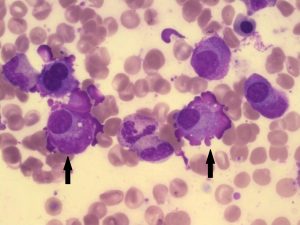
- An image from a bone marrow direct smear from a patient with plasma cell myeloma demonstrating two plasma cells (indicated by arrows). 50x oil immersion. From MLS Collection, University of Alberta, https://doi.org/10.7939/R3348GX60
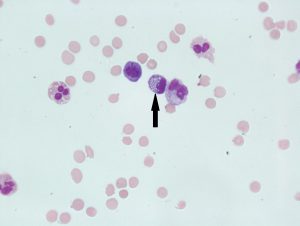
- An image from a fluid cytospin slide showing a mott cell (indicated with an arrow) with round globules (Russell bodies). Mott cells may also be seen in plasma cell myeloma bone marrow smears. 60X oil immersion. From MLS Collection, University of Alberta, https://doi.org/10.7939/R3RV0DG30
- An image from a fluid cytospin slide demonstrating a mott cell (indicated with an arrow) with round globules (Russell bodies). Mott cells may be seen in plasma cell myeloma bone marrow smears. 60X oil immersion. From MLS Collection, University of Alberta, https://doi.org/10.7939/R31C1TX1V
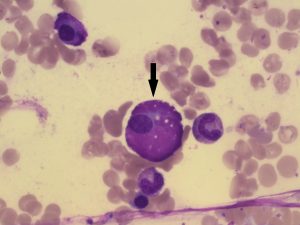
- An image from a bone marrow direct smear from a patient with plasma cell myeloma demonstrating a large plasma cell variant known as a flame cell (indicated by an arrow). 100x oil immersion. From MLS Collection, University of Alberta, https://doi.org/10.7939/R3CF9JN7P
- An image from a bone marrow direct smear from a patient with plasma cell myeloma demonstrating a large plasma cell variant known as a flame cell (indicated by arrows). 100x oil immersion. From MLS Collection, University of Alberta, https://doi.org/10.7939/R3416TF3X
Features:
This disorder is characterized by an increase in M protein (monoclonal gammopathy) in the serum and/or urine with the presence of clonal plasma cells in the bone marrow.1
Unlike MGUS, patients with plasma cell myeloma often present with CRAB symptoms (hyperCalcemia, Renal failure, Anemia, and lytic Bone lesions). Additional features include osteolytic bone lesions without new bone formation.1,2 Some patients may be asymptomatic (smoldering multiple myeloma) but other findings of plasma cell myeloma may still be found.1,3
Due to bone damage, extramedullary hematopoiesis is a common finding.1
Cause:
Most cases of plasma cell myeloma have developed from MGUS.2
Other causes include infections, exposure to toxic substances, and other chronic diseases which may result in a long term antigenic stimulation.1
Cytogenetic abnormalities have been found to be associated with the development of multiple myeloma.3
Age Group Affected: >50 years old, more common in males.1
Plasma Cell Morphology:
Aside from the characteristic appearance of plasma cells, morphologic variants of plasma cells are often seen in Plasma Cell Myeloma. These include bi-lobed plasma cells, flame cells, and mott cells.
Flame Cells:
A reactive plasma cell that has reddish-purple cytoplasms. Colour of the cytoplasm is caused by glycoprotein and ribosomes. The presence of flame cells has been associated with IgA multiple myeloma.4
Mott Cells:
Are plasma cells with multiple round inclusions in the cytoplasm. The inclusions are termed “Russell bodies” and are composed of immunoglobulins.3
Laboratory Results for Plasma Cell Myeloma:1,2
|
CBC: Cytopenias due to decreased bone marrow hematopoiesis RBC: Decreased HB: Decreased |
PBS: Rouleaux formation (Due to M protein) Rare circulating plasma cells Normocytic Normochromic |
BM: Lytic regions Plasmacytosis (>10%) Bi-lobed plasma cells, Flame cells, and/or Mott cells may be seen. Biopsy: interstitial clusters of plasma cells Aspirates: shows various heterogeneous forms of plasma cells in aggregates or sheets. |
|
Immunologic Markers: CD38, CD79a, CD138 |
Other Tests: Serum FLC: Increased Bence-Jones proteinuria FISH Protein electrophoresis Immunofixation FLC assays Cytogenetics |
Reactive Plasmacytosis:
An increase in the number plasma cells and immunoglobulins can also be the result of a non-malignant condition. Bacterial and viral infections (e.g infections mononucleosis, tuberculosis) can evoke a strong antigenic response and lead to an increase in plasma cells in the peripheral blood.4 The reactive process should NOT be confused with plasma cell myeloma.
Unlike plasma cell myeloma, there are no findings of CRAB symptoms or clonal plasma cells in the bone marrow. Plasma cells may be increased in the bone marrow, but not above 10% . An increase in M proteins and plasma cells (outside the bone marrow) may be found.3
References:
1. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. editors. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues Volume 2. 4th ed. International Agency for Research on Cancer (IARC); 2008.
2. Rajkumar SV. Multiple myeloma: 2016 update on diagnosis, risk-stratification, and management. Am J Hematol [Internet]. 2016 Jul [cited 2018 Jun 27];91(7):719–34. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5291298/
3. Craig F. Mature lymphoid neoplasms. In: Clinical laboratory hematology. 3rd ed. New Jersey: Pearson; 2015. p. 535-56.
4. Beglinger SS. Nonmalignant lymphocyte disorders. In: Clinical laboratory hematology. 3rd ed. New Jersey: Pearson; 2015. p. 409-24.